Key Takeaways
- Piles are swollen veins in or around the anus that can cause itching, pain, or bleeding.
- Knowing the types and causes helps you recognize symptoms early and manage them effectively.
- Simple lifestyle changes and proper treatment can relieve discomfort and prevent recurrence.
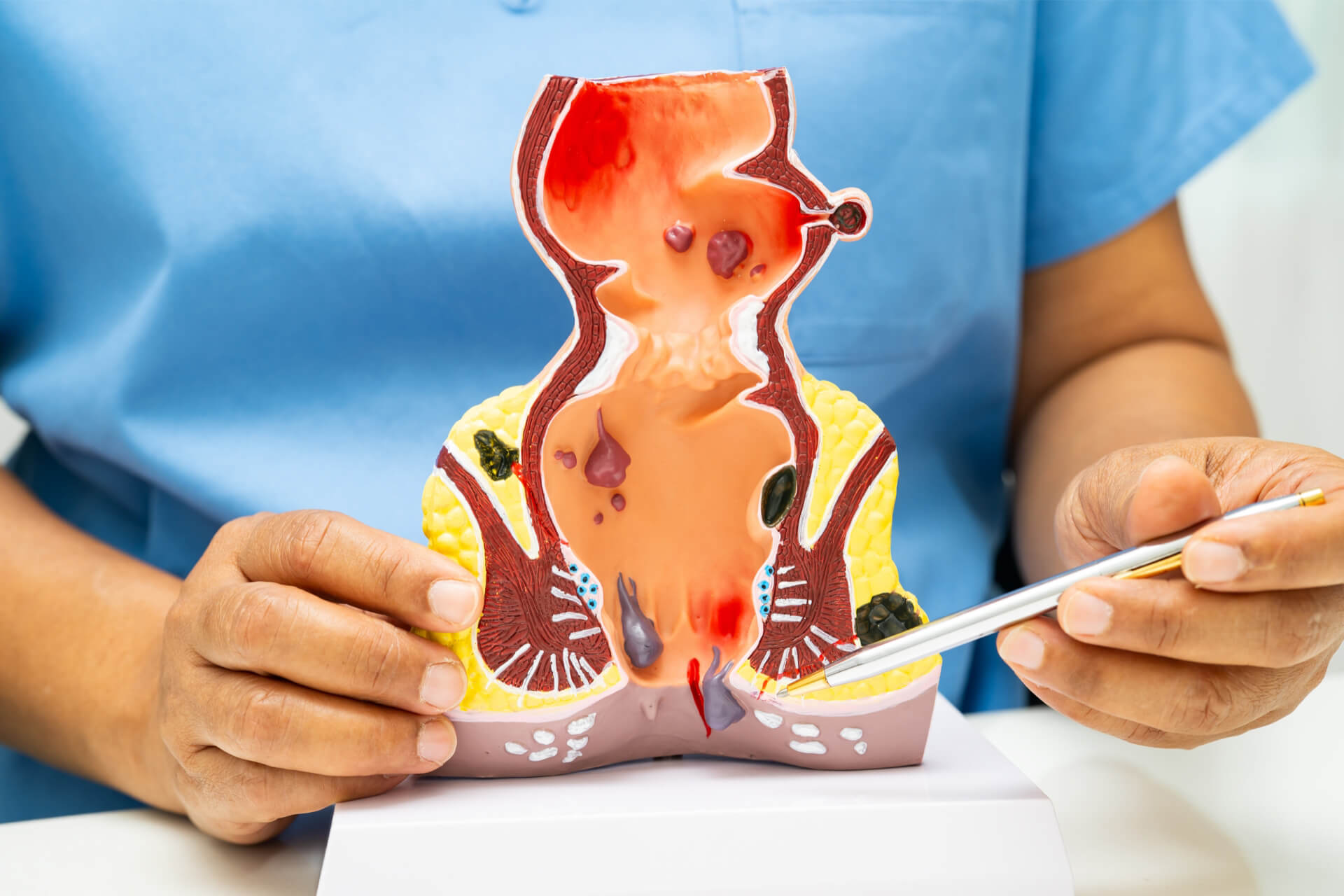
Piles, also known as hemorrhoids, can cause discomfort, itching, or bleeding around the anus. You might notice them after straining during bowel movements or sitting for long periods. Piles are swollen veins that develop inside or around your bottom and can often be managed with simple lifestyle changes and treatments.
You can have internal piles that form inside the rectum or external piles that develop under the skin around the anus. Each type can cause different symptoms, ranging from mild irritation to painful swelling. Understanding what triggers them helps you prevent flare-ups and find relief faster.
With the right approach, you can ease pain, reduce inflammation, and prevent piles from returning. From increasing fiber in your diet to knowing when to seek medical advice, learning how to manage piles puts you in control of your comfort and health.
Contents
1. Understanding Piles (Hemorrhoids)
- What Are Hemorrhoids?
- Anatomy of the Anus and Rectum
- The Key Difference: Internal vs. External Hemorrhoids
2. Types of Piles and Their Characteristics
3. Common Symptoms and Warning Signs
- Chronic Constipation and Straining
- Diarrhea and Bowel Habits
- Dietary Influences
- Lifestyle and Genetic Factors
Understanding Piles (Hemorrhoids)
Piles, or hemorrhoids, develop when veins in your rectum or anus swell due to increased pressure or strain. They can form internally or externally and often cause discomfort, itching, or bleeding during bowel movements. Recognizing where and how they form helps you understand symptoms and choose effective relief methods.
What Are Hemorrhoids?
Hemorrhoids are swollen vascular structures in the lower rectum and anus. In their normal state, these veins act as cushions that help control stool passage. When they become enlarged or inflamed, they are referred to as piles.
You may experience bleeding, irritation, or pain depending on the type and severity. Internal hemorrhoids often bleed painlessly, while external ones can cause tenderness or swelling around the anal opening.
Common causes include chronic constipation, prolonged sitting, pregnancy, and straining during bowel movements. These factors increase pressure in the rectal veins, leading to vein dilation. While hemorrhoids are common, they are not usually dangerous and often respond well to conservative management such as dietary changes and proper hygiene.
Anatomy of the Anus and Rectum
Your rectum connects the large intestine to the anus, serving as a temporary storage area for stool. The anus is the muscular opening that allows stool to exit the body. Both areas contain a network of blood vessels, connective tissue, and muscles that maintain continence.
The hemorrhoidal plexus, a group of veins in the anal canal, plays a key role in hemorrhoid formation. When pressure builds, these veins stretch and bulge, forming internal or external hemorrhoids.
Proper function of the internal and external anal sphincters ensures controlled stool release. Weakness, irritation, or repeated strain in this region can disrupt normal circulation, contributing to hemorrhoid development. Understanding this structure helps explain why sitting for long periods or straining can worsen symptoms.
The Key Difference: Internal vs. External Hemorrhoids
| Type: Internal | |
|---|---|
| Location | Inside the rectum |
| Common Symptoms | Bright red bleeding, prolapse |
| Pain Level | Usually painless |
| Type: External | |
|---|---|
| Location | Under the skin around the anus |
| Common Symptoms | Itching, swelling, discomfort |
| Pain Level | Often painful |
Internal hemorrhoids form inside the rectum and are typically not visible or painful unless they prolapse. You might notice blood on toilet paper or in the bowl after a bowel movement.
External hemorrhoids develop beneath the skin around the anus, where many pain-sensitive nerves exist. When irritated or thrombosed, they can cause sharp pain and noticeable lumps.
Both types can coexist, and their symptoms may overlap. Identifying which type you have helps guide treatment—ranging from simple lifestyle adjustments to medical procedures when needed.
Types of Piles and Their Characteristics
Piles vary depending on where they develop and how severely the veins are affected. Each type presents distinct symptoms, levels of discomfort, and treatment needs that influence how you manage daily activities and seek medical care.

Internal Hemorrhoids
Internal hemorrhoids form inside your rectum, where pain-sensing nerves are limited. You may not feel them at first, but they can cause bleeding during bowel movements or leave mucus on toilet paper.
They are often graded from I to IV based on how far they protrude from the anus:
| Grade: I | |
|---|---|
| Description | Remain inside the rectum |
| Grade: II | |
|---|---|
| Description | Prolapse but retract on their own |
| Grade: III | |
|---|---|
| Description | Prolapse and require manual pushing back |
| Grade: IV | |
|---|---|
| Description | Permanently prolapsed and cannot be reinserted |
Mild cases often improve with fiber intake, hydration, and topical treatments. More advanced grades may require medical procedures like rubber band ligation or sclerotherapy.
External Hemorrhoids
External hemorrhoids develop under the skin around your anus. Because this area contains many nerves, they tend to cause more pain and irritation than internal hemorrhoids.
You may notice swelling, itching, or small lumps near the anal opening. Sitting or straining during bowel movements can make the discomfort worse. The affected veins may appear bluish or purplish due to trapped blood.
Keeping the area clean, using a warm Sitz bath, and applying over-the-counter creams can relieve symptoms. In persistent cases, a doctor may recommend minor surgical removal to prevent recurrent inflammation.
Thrombosed Hemorrhoids
A thrombosed hemorrhoid occurs when a blood clot (thrombus) forms inside an external or internal hemorrhoid. This clot causes sudden, sharp pain, swelling, and sometimes a dark bluish lump around the anus.
Pain is often most intense within the first 48 to 72 hours. The clot may gradually dissolve, but the area can remain tender. If untreated, the clot can break down, leading to skin irritation or ulceration.
Medical treatment may involve a small incision to remove the clot if addressed early. Otherwise, conservative care with pain relief and warm baths helps the tissue heal naturally over time.
Prolapsed Hemorrhoids
Prolapsed hemorrhoids are internal hemorrhoids that extend outside the anus due to pressure or straining. They may retract on their own or require gentle manual repositioning.
You might notice soft, moist lumps that become irritated or painful after bowel movements. The tissue can swell and cause bleeding, itching, or mucus discharge.
Doctors classify prolapsed hemorrhoids by severity, from those that retract easily to those that remain permanently outside. Treatments range from dietary adjustments and topical medications to surgical correction for severe or persistent cases.
Common Symptoms and Warning Signs
You may notice bleeding during bowel movements, irritation around the anus, or a feeling of fullness or swelling. These changes often indicate inflammation or pressure on the veins in the rectal area and can vary in severity depending on the type and stage of hemorrhoids.

Rectal Bleeding
Rectal bleeding is one of the most frequent signs of hemorrhoids. You might see bright red blood on toilet paper, in the toilet bowl, or on the surface of the stool. The color usually indicates that the bleeding originates from the lower rectum rather than higher in the digestive tract.
Bleeding often occurs after straining or passing hard stool. In most cases, it is mild and stops on its own. However, persistent or heavy bleeding can signal complications such as anemia or another condition that requires medical evaluation.
You should seek medical advice if bleeding continues for more than a few days, becomes heavy, or is accompanied by dark or tarry stools, which may indicate bleeding from another source.
Anal Itching and Discomfort
Anal itching, also called pruritus ani, is common with both internal and external hemorrhoids. The itching often results from mucus leakage, moisture, or irritation of the surrounding skin. You may also feel a burning sensation or mild soreness after bowel movements.
Scratching the area can worsen irritation and lead to small skin breaks or infection. To reduce discomfort, keep the anal area clean and dry. Using unscented wipes or gentle cleansing with warm water can help prevent further irritation.
If itching persists despite good hygiene, a healthcare provider may recommend a mild corticosteroid cream or barrier ointment to calm inflammation and protect the skin.
Mucus Discharge
Internal hemorrhoids can produce a clear or slightly yellow mucus discharge. This discharge may appear on underwear or toilet tissue and often accompanies a feeling of incomplete evacuation after a bowel movement.
Mucus leakage can irritate the surrounding skin, leading to itching or mild inflammation. Using breathable cotton underwear and changing it regularly helps reduce moisture buildup.
While a small amount of mucus is common, excessive or persistent discharge—especially if mixed with blood or pus—should be evaluated by a doctor. These symptoms can occasionally overlap with other rectal conditions such as infections or inflammatory bowel disease.
Pain and Swelling
Pain and swelling are more common with external hemorrhoids or when a blood clot forms inside a swollen vein, known as a thrombosed hemorrhoid. This can cause a firm, tender lump near the anus and sudden, sharp pain during sitting or bowel movements.
Swelling may also cause a sensation of fullness or pressure. Applying a cold compress or taking a warm sitz bath can help reduce inflammation and discomfort.
If pain becomes severe or swelling does not improve within a few days, medical treatment such as clot removal or prescription medication may be necessary to relieve symptoms and prevent further irritation.
Causes and Risk Factors
Piles develop when pressure increases in the veins of your rectum and anus, making them swell and sometimes protrude. Everyday habits, bowel patterns, and diet play a major role in how these veins respond to strain and pressure.

Chronic Constipation and Straining
Chronic constipation is one of the most frequent triggers of hemorrhoids. When you strain during bowel movements, you raise the pressure inside the lower rectum, which can enlarge the veins and weaken the surrounding tissue. Over time, this repeated stress can lead to internal or external piles.
You can reduce this risk by keeping stools soft and avoiding prolonged sitting on the toilet. Drinking enough fluids and including fiber-rich foods such as fruits, vegetables, and whole grains helps maintain regularity. If constipation persists, your healthcare provider may suggest a stool softener or mild laxative.
| Helpful Habits: Drink 6–8 glasses of water daily | |
|---|---|
| Why They Matter | Keeps stools soft |
| Helpful Habits: Eat fiber-rich foods | |
|---|---|
| Why They Matter | Reduces straining |
| Helpful Habits: Avoid delaying bowel movements | |
|---|---|
| Why They Matter | Prevents stool hardening |
Diarrhea and Bowel Habits
Frequent diarrhea can irritate the anal area and cause inflammation. Repeated wiping and the passage of loose stools increase friction and pressure on the veins around the anus. This can lead to swelling similar to that caused by constipation.
Irregular bowel habits—alternating between diarrhea and constipation—also strain the rectal veins. You can help prevent irritation by treating underlying digestive issues and maintaining consistent bowel routines. Using soft, unscented toilet paper or rinsing gently with water can reduce irritation after bowel movements.
Keeping a record of your bowel patterns may help identify triggers such as certain foods, stress, or medications. Addressing these triggers early can prevent flare-ups and discomfort.
Dietary Influences
Your diet has a direct impact on bowel function and stool consistency. A low-fiber diet often leads to hard stools and constipation, increasing the need to strain. Conversely, a high-fiber diet improves stool bulk and softness, reducing the risk of hemorrhoids.
Fiber sources include oats, beans, lentils, berries, and leafy greens. Gradually increasing fiber intake prevents gas and bloating. Pairing fiber with adequate water intake helps the digestive system move waste efficiently.
Limiting processed foods, refined grains, and excess salt can also help. These foods may slow digestion or contribute to dehydration, both of which make bowel movements more difficult.
Lifestyle and Genetic Factors
Your daily habits and family history can influence your likelihood of developing piles. Sitting or standing for long periods increases pressure in the rectal veins. A sedentary lifestyle slows bowel function, while regular physical activity promotes healthy digestion.
Pregnancy, obesity, and aging also raise the risk by adding pressure to the pelvic area or weakening connective tissues. If hemorrhoids run in your family, you may be more prone to them due to inherited vein structure or tissue strength.
You can lower your risk by staying active, maintaining a healthy weight, and avoiding prolonged sitting. Even simple actions—like walking after meals or using a footstool during bowel movements—can improve circulation and reduce strain.
Diagnosis and Medical Evaluation
Accurate diagnosis helps identify the cause of rectal bleeding, pain, or swelling and ensures you receive the right treatment. Evaluation often involves a combination of physical assessment and visual inspection of the anal canal and rectum using specific instruments.

Physical Examination and Rectal Exam
Your healthcare provider begins by reviewing your symptoms, including bleeding, pain, or prolapse. A physical examination follows, usually with you lying on your side in a relaxed position.
The doctor inspects the perianal area for external hemorrhoids, skin tags, fissures, or swelling. A digital rectal exam involves gently inserting a lubricated, gloved finger into your rectum to assess tone, tenderness, and the presence of internal masses.
This exam helps evaluate whether hemorrhoids are internal or external and rules out other causes like tumors or abscesses. You may feel mild pressure but not significant pain. The findings guide whether further tests are needed.
Anoscopy and Colonoscopy
If internal hemorrhoids are suspected, your doctor may perform an anoscopy. This procedure uses a short, hollow tube with a light to view the lower rectum and anal canal. It helps confirm the grade of internal hemorrhoids and detect inflammation or bleeding sites.
Anoscopy is quick and typically done in the office without anesthesia. It provides direct visualization of tissue that cannot be seen during a standard rectal exam.
When symptoms include persistent bleeding, anemia, or risk factors for colorectal disease, a colonoscopy may be recommended. This test examines the entire colon using a flexible camera to rule out polyps, cancer, or inflammatory bowel disease.
| Procedure: Digital Rectal Exam | |
|---|---|
| Purpose | Detects masses, tone, tenderness |
| Setting | Office |
| Sedation | No |
G
| Procedure: Anoscopy | |
|---|---|
| Purpose | Visualizes anal canal |
| Setting | Office |
| Sedation | No |
| Procedure: Colonoscopy | |
|---|---|
| Purpose | Examines colon and rectum |
| Setting | Endoscopy unit |
| Sedation | Yes |
Differentiating from Other Conditions
Rectal bleeding and discomfort may result from several conditions beyond hemorrhoids. Common alternatives include anal fissures, rectal prolapse, polyps, and colorectal cancer.
Your doctor distinguishes these by evaluating bleeding patterns, pain characteristics, and exam findings. For example, fissures often cause sharp pain during bowel movements, while hemorrhoidal bleeding is usually painless and bright red.
Laboratory tests or imaging may be used if symptoms remain unclear. Accurate differentiation prevents unnecessary treatment and ensures that serious conditions are not overlooked.
Relief, Treatment, and Prevention Strategies
You can relieve hemorrhoid symptoms and prevent recurrence through consistent self-care, proper diet, and evidence-based medical treatment. The best approach depends on symptom severity, hemorrhoid type, and how well you respond to conservative or procedural care.

Home Remedies and Lifestyle Changes
Simple daily habits often bring the most lasting relief. Increasing dietary fiber through foods like whole grains, fruits, and vegetables or using fiber supplements such as psyllium helps soften stool and reduce straining. Drinking adequate water—about 1.5 to 2 liters per day—supports this effect.
A sitz bath (sitting in warm water for 10–15 minutes several times a day) can soothe itching and swelling. You can use plain warm water without additives. Practicing good anal hygiene and gently patting the area dry prevents irritation.
Avoid sitting for long periods and maintain regular physical activity to promote bowel regularity. Using a stool softener or mild laxative may help if constipation persists. Limiting caffeine and alcohol can also reduce dehydration-related constipation.
Over-the-Counter and Prescription Treatments
Topical over-the-counter creams, ointments, and suppositories containing hydrocortisone, lidocaine, or witch hazel can temporarily ease itching and discomfort. Apply them as directed for short periods to avoid skin thinning or irritation.
If symptoms persist, your clinician may prescribe stronger topical corticosteroids or vasoactive agents that improve venous tone. Oral flavonoid-based medications can also reduce bleeding and swelling in some cases.
You should avoid frequent use of harsh cleansing wipes or perfumed products, which can worsen irritation. When pain is significant, mild analgesics such as acetaminophen may help, but avoid nonsteroidal anti-inflammatory drugs if bleeding is present.
Minimally Invasive Procedures
When conservative care fails, office-based procedures can treat internal hemorrhoids effectively with minimal downtime. Rubber band ligation (RBL) is the most common method; it cuts off blood flow to the hemorrhoid, causing it to shrink and fall off within days.
Sclerotherapy involves injecting a chemical solution—such as polidocanol foam—into the hemorrhoidal tissue to cause it to collapse and scar. Infrared coagulation and electrocoagulation use heat or electrical energy to coagulate vessels and shrink tissue.
These procedures are typically performed without general anesthesia and allow you to return to normal activities quickly. Mild pain or bleeding may occur for a few days afterward, but serious complications are rare when performed by experienced clinicians.
Surgical Options for Severe Cases
If you have large, prolapsed, or recurrent hemorrhoids that do not respond to other treatments, surgery may be necessary. Hemorrhoidectomy—the surgical removal of hemorrhoidal tissue—remains the most definitive option for grades III and IV hemorrhoids. It effectively prevents recurrence but requires a longer recovery period and carries risks such as pain, bleeding, or anal stenosis.
Stapled hemorrhoidopexy (also called stapled hemorrhoid surgery) repositions prolapsed tissue and interrupts blood flow using a circular stapling device. It generally causes less postoperative pain than traditional excision but may have a higher chance of recurrence.
Your surgeon will recommend the most suitable approach based on hemorrhoid grade, symptom severity, and your overall health. Careful postoperative hygiene, pain management, and stool softening reduce complications and support healing.

