Key Takeaways
- HSV-1 and HSV-2 are lifelong infections with distinct but overlapping patterns.
- Early diagnosis and antiviral treatment help control outbreaks and transmission.
- Awareness of triggers and safe practices reduces recurrence and spread.
Understanding herpes simplex helps you take control of your health with clarity and confidence. Two main types—HSV-1 and HSV-2—cause similar infections that can appear around the mouth or genitals, yet they differ in how they spread and how often they recur. Both forms are manageable with proper care, medication, and awareness of how the virus behaves in your body.
You may already carry HSV without symptoms, as many people do. When outbreaks occur, they often cause small, painful blisters or sores that heal within days to weeks. Recognizing early signs and starting antiviral treatment quickly can shorten outbreaks, reduce discomfort, and lower the risk of transmission.
Learning how HSV spreads and what triggers flare-ups helps you protect yourself and others. With the right information and medical support, you can manage symptoms effectively and maintain a healthy, confident life.

Vaccination Program
Explore our range of vaccination programs designed for your specific health needs.
Herpes Simplex Virus Overview
Herpes simplex virus (HSV) is a common, lifelong infection that affects billions of people worldwide. It spreads mainly through direct contact with infected skin or bodily fluids and can cause either oral or genital symptoms depending on the virus type. With proper care and treatment, you can manage symptoms and reduce transmission risk.
What Is Herpes Simplex
Herpes simplex refers to a group of viral infections caused by the herpes simplex virus (HSV). The virus belongs to the Herpesviridae family and is characterized by its ability to remain dormant in nerve cells after the initial infection.
Once infected, you may experience blisters, ulcers, or tingling sensations near the affected area. These symptoms often appear during an outbreak and may recur over time.
HSV spreads through skin-to-skin contact, including kissing, oral contact, or sexual activity. Even without visible sores, the virus can still transmit because it sheds from the skin intermittently.
While herpes cannot be cured, antiviral medications such as acyclovir, valacyclovir, and famciclovir help shorten outbreaks, ease discomfort, and lower the chance of spreading the virus to others.
Types of Herpes Viruses
There are two main types of herpes simplex virus: HSV-1 and HSV-2.
| Type: HSV-1 | |
|---|---|
| Common Infection Site | Mouth and lips (oral herpes) |
| Main Transmission Route | Oral contact, kissing, sharing utensils |
| Typical Symptoms | Cold sores, fever blisters |
| Type: HSV-2 | |
|---|---|
| Common Infection Site | Genital and anal areas (genital herpes) |
| Main Transmission Route | Sexual contact |
| Typical Symptoms | Genital blisters, sores, pain |
HSV-1 usually causes oral herpes but can also affect the genitals through oral-genital contact. HSV-2 primarily causes genital herpes and tends to recur more frequently.
Both viruses can be transmitted when no symptoms are visible. You can reduce risk by avoiding contact during outbreaks and using barrier protection such as condoms or dental dams.
Prevalence and Epidemiology
Herpes simplex infections are widespread across all regions and age groups. According to global estimates, about two-thirds of people under 50 carry HSV-1, while around 13% of adults aged 15–49 have HSV-2.
HSV-1 is often acquired in childhood through nonsexual contact. HSV-2 typically spreads later in life through sexual activity. Women are affected more often than men because transmission from men to women occurs more easily.
Infection rates rise with age, but most new cases occur among adolescents and young adults. Many people never notice symptoms, which contributes to ongoing transmission. Understanding your infection status and practicing preventive measures can help protect both you and your partners.
HSV-1 vs. HSV-2: Key Differences
Both herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) share similar structures and behaviors but differ in where they usually appear, how often they recur, and how they spread. Understanding these distinctions helps you recognize symptoms early and manage the condition more effectively.

Genetic and Structural Differences
HSV-1 and HSV-2 are closely related members of the Herpesviridae family. Each contains double-stranded DNA enclosed in a protein shell and lipid envelope. Despite their genetic similarity—about 50% DNA sequence overlap—they differ enough to influence how your immune system responds.
HSV-1 typically establishes latency in the trigeminal ganglia near the face, while HSV-2 favors the sacral ganglia near the spine. This difference in nerve location partly determines where outbreaks occur.
Both viruses can infect either the oral or genital area, but their genetic variations affect replication rate and shedding frequency. HSV-2 tends to shed more frequently and for longer periods, increasing its likelihood of transmission during sexual contact.
| Feature: Genome similarity | |
|---|---|
| HSV-1 | ~50% shared DNA |
| HSV-2 | ~50% shared DNA |
| Feature: Latency site | |
|---|---|
| HSV-1 | Trigeminal ganglia (head/neck) |
| HSV-2 | Sacral ganglia (lower spine) |
| Feature: Shedding frequency | |
|---|---|
| HSV-1 | Lower |
| HSV-2 | Higher |
Typical Infection Sites
HSV-1 most often causes oral herpes, producing cold sores or blisters around your mouth or lips. It spreads mainly through oral contact, such as kissing or sharing utensils. However, it can also cause genital herpes through oral–genital contact.
HSV-2 primarily causes genital herpes, affecting the genital and anal areas. It spreads almost exclusively through sexual contact. Because HSV-2 is adapted to the genital region, it tends to cause more frequent and symptomatic outbreaks there.
Although both viruses can infect either site, the likelihood of recurrence and viral shedding is influenced by the infection’s location. For example, genital HSV-1 infections usually recur less often and shed less virus than genital HSV-2 infections.
Patterns of Recurrence
After your first infection, both HSV-1 and HSV-2 remain dormant in nerve cells and can reactivate later. The rate and intensity of recurrence differ between the two.
HSV-2 tends to reactivate more regularly, often several times per year, especially during periods of stress, illness, or immune suppression. HSV-1 reactivates less frequently, particularly when it affects the genitals.
You may notice early warning signs called prodromal symptoms—tingling, itching, or mild pain—before lesions appear. Antiviral medications such as acyclovir, valacyclovir, or famciclovir can reduce recurrence frequency and viral shedding, helping you manage symptoms and lower transmission risk.
While neither virus leaves your body after infection, consistent treatment and preventive measures can help you maintain control and reduce the impact on your daily life.
Transmission and Risk Factors
Herpes simplex virus spreads through direct contact with infected skin or bodily fluids. You can reduce your risk by understanding how the virus transmits, what behaviors increase exposure, and the situations that make infection more likely.

Modes of Transmission
You can contract herpes simplex virus type 1 (HSV‑1) or type 2 (HSV‑2) through skin‑to‑skin or mucous membrane contact. HSV‑1 typically spreads through oral contact, such as kissing or sharing utensils, while HSV‑2 mainly spreads through sexual contact involving the genitals or anus.
Transmission can occur even when no visible sores are present. The virus sheds from normal‑appearing skin, which means protection methods like condoms lower but do not eliminate risk.
Common routes of spread include:
- Kissing or oral contact (HSV‑1)
- Genital or anal sex (HSV‑2)
- Contact with saliva or genital fluids
Avoid touching sores and then other body parts, as autoinoculation can transfer the virus to new sites, such as the eyes or fingers.
Role of Oral Sex
Oral sex can transmit either HSV‑1 or HSV‑2 between the mouth and genitals. When a partner with oral herpes performs oral sex, HSV‑1 can cause genital herpes. Conversely, HSV‑2 may pass from the genitals to the mouth.
Because HSV can shed without visible symptoms, infection may happen even when neither partner notices sores. Using condoms or dental dams during oral sex lowers, but does not completely prevent, transmission.
You can further reduce risk by avoiding oral contact during active outbreaks and by not sharing items that come into contact with saliva, such as lip balm or eating utensils. Regular communication with partners about symptoms and testing helps prevent unintentional spread.
Risk Factors for Infection
Several factors increase your likelihood of acquiring herpes infection. Sexual activity without barrier protection is the primary risk, especially with multiple partners. HSV‑2 transmission is more efficient from men to women, making women statistically more affected worldwide.
Other risk factors include:
| Risk Factor: Early sexual activity | |
|---|---|
| Explanation | More years of potential exposure |
| Risk Factor: History of other STIs | |
|---|---|
| Explanation | Damaged mucous membranes increase susceptibility |
| Risk Factor: Weakened immune system | |
|---|---|
| Explanation | Reduces ability to suppress viral replication |
| Risk Factor: Unawareness of partner’s infection | |
|---|---|
| Explanation | Asymptomatic shedding leads to unnoticed spread |
Using condoms, limiting partners, and considering daily antiviral therapy if you have frequent outbreaks can help reduce transmission risk.
Mother-to-Child Transmission
Herpes can pass from mother to baby during childbirth, known as neonatal herpes. This occurs when the infant contacts the virus in the birth canal, especially if the mother acquires a new infection late in pregnancy.
Neonatal herpes is rare but serious. It can affect the infant’s skin, eyes, or nervous system. You should inform your healthcare provider if you have a history of herpes or develop symptoms while pregnant.
To lower transmission risk, your provider may recommend antiviral medication in the final weeks of pregnancy or a cesarean delivery if active genital lesions are present at labor. Early management protects both you and your baby from complications.
Symptoms and Clinical Presentation
Herpes simplex virus infections can appear in different ways depending on the site of infection and whether it is a first episode or recurrence. You may notice visible sores or experience few or no symptoms at all, yet the virus can still be active and transmissible.

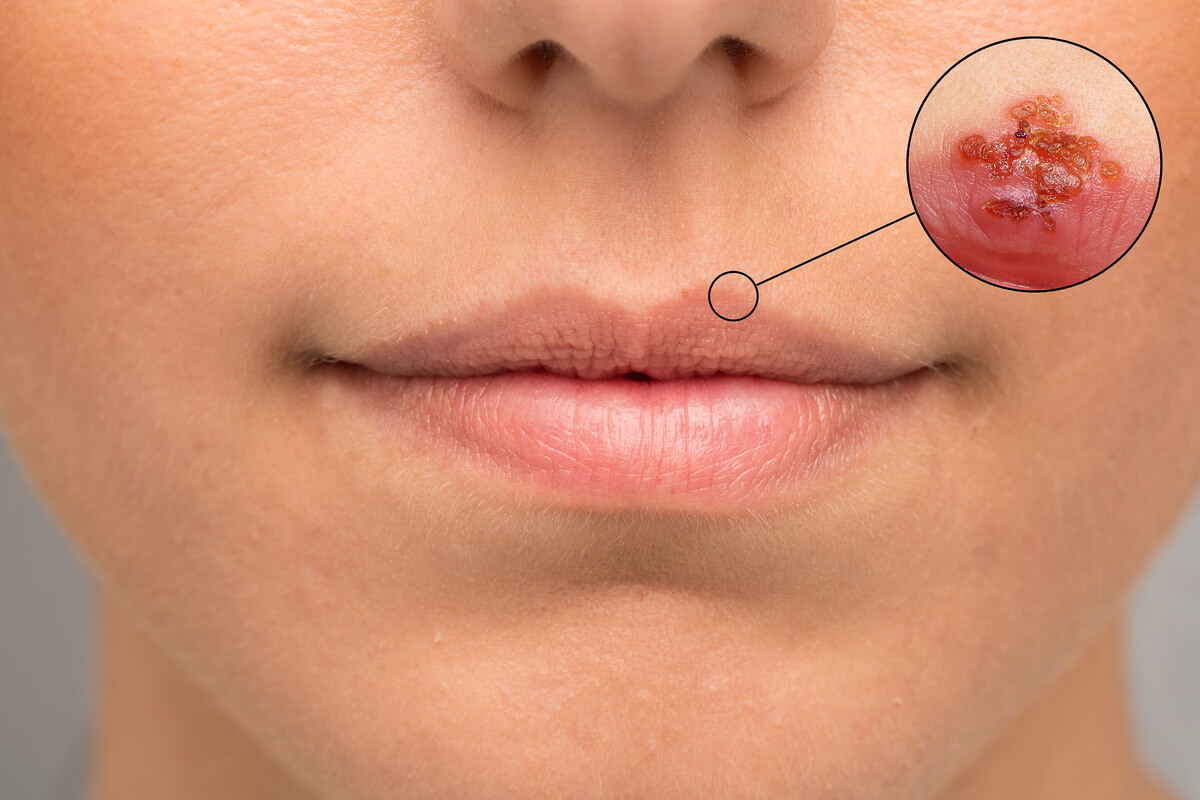
Oral Herpes Symptoms
Oral herpes, usually caused by HSV‑1, often presents as cold sores or fever blisters around the lips or mouth. These lesions may start with tingling, itching, or burning before small fluid‑filled blisters appear.
The blisters can break open, ooze, and crust over within several days. Pain or discomfort is common, especially during the first episode. You might also experience fever, sore throat, or swollen lymph nodes during an initial outbreak.
Recurrences are generally milder and shorter. Triggers such as sunlight, stress, or illness can reactivate the virus. Applying sunscreen to the lips and managing stress may help reduce future episodes.
| Common Oral Herpes Signs: Tingling or burning | |
|---|---|
| Description | Early warning before sores appear |
| Common Oral Herpes Signs: Clusters of blisters | |
|---|---|
| Description | Usually on or around lips |
| Common Oral Herpes Signs: Crusting lesions | |
|---|---|
| Description | Healing stage of cold sores |
Genital Herpes Symptoms
HSV‑2 most often causes genital herpes, though HSV‑1 can also infect this area through oral‑genital contact. You may first feel itching, tenderness, or burning in the genital or anal region before herpes sores appear.
These sores can form as blisters that rupture into shallow ulcers. They may cause pain when you urinate or during sexual activity. The first outbreak often includes fever, body aches, or swollen lymph nodes.
Recurrent episodes tend to be less severe and heal within one to two weeks. Suppressive antiviral therapy can reduce the frequency and intensity of these outbreaks.
| Common Genital Herpes Signs: Painful genital sores | |
|---|---|
| Description | Blisters or ulcers on genitals or anus |
| Common Genital Herpes Signs: Local itching or burning | |
|---|---|
| Description | Often precedes visible lesions |
| Common Genital Herpes Signs: Flu-like symptoms | |
|---|---|
| Description | Fever, fatigue, swollen glands during first episode |
Atypical and Asymptomatic Cases
Many people with herpes never develop visible sores. You may carry the virus without knowing and still shed it intermittently, which can transmit infection to others.
Atypical symptoms can include mild itching, small fissures, or redness mistaken for irritation or another skin condition. These subtle signs can make diagnosis difficult without laboratory testing.
Because asymptomatic shedding is common, using protection and avoiding contact during any unusual sensations can help lower risk. A blood test or swab can confirm infection even when sores are absent.
Complications of Herpes
Complications are uncommon but can occur, particularly if your immune system is weakened. HSV‑2 infection may increase the risk of acquiring or transmitting HIV.
Severe cases can involve widespread skin lesions or, rarely, infection of the brain (encephalitis) or eyes (keratitis). Pregnant individuals with new genital herpes near delivery risk passing the virus to the newborn, leading to neonatal herpes.
Prompt medical evaluation and antiviral treatment reduce these risks. Regular follow‑up with your healthcare provider supports safe management and helps prevent complications.
Diagnosis and Testing
Accurate diagnosis of herpes simplex virus (HSV) helps guide treatment, prevent transmission, and reduce uncertainty. Testing identifies whether HSV-1 or HSV-2 is present and distinguishes between an active infection and past exposure.

Clinical Evaluation
A healthcare provider begins by assessing visible signs and your medical history. Common findings include blisters, ulcers, or crusted lesions on the mouth, genitals, or surrounding skin.
You may be asked about the timing, frequency, and duration of symptoms, as well as any known exposure to HSV. Because herpes symptoms can resemble other skin conditions, such as syphilis or eczema, clinical evaluation alone cannot confirm the diagnosis.
During an active outbreak, your provider may collect a swab from a lesion for laboratory testing. This step ensures that the diagnosis is based on direct evidence rather than visual inspection alone.
Laboratory Testing Methods
Laboratory testing confirms HSV infection using samples from sores, mucosal surfaces, or blood. The main diagnostic methods include viral culture, polymerase chain reaction (PCR), and antibody testing.
A viral culture involves growing the virus from a swabbed sample in a controlled environment. While specific, it can take several days and may miss infections if lesions are healing.
Modern testing often favors molecular techniques like PCR for speed and accuracy. These methods detect viral DNA even when symptoms are mild or absent. Blood-based tests that detect antibodies are used when no active lesions are available for sampling.
| Method: Viral culture | |
|---|---|
| Detects | Live virus |
| Typical Use | Active lesions |
| Turnaround Time | 2–14 days |
| Method: PCR | |
|---|---|
| Detects | Viral DNA |
| Typical Use | Active or latent infection |
| Turnaround Time | 1–2 days |
| Method: Serology | |
|---|---|
| Detects | Antibodies |
| Typical Use | Past or recent infection |
| Turnaround Time | 1–3 days |
Polymerase Chain Reaction (PCR)
PCR testing identifies HSV DNA directly from lesion swabs, cerebrospinal fluid, or other samples. It is highly sensitive and specific, making it the preferred method for diagnosing active herpes infection.
PCR can distinguish between HSV-1 and HSV-2, which helps guide counseling and treatment decisions. It also detects viral shedding, even when no visible lesions are present, allowing for more accurate assessment of transmission risk.
Because PCR amplifies genetic material, even small amounts of virus can be detected. This makes it useful in complex cases, such as neonatal herpes or suspected herpes encephalitis, where early confirmation is crucial for care.
Antibody Testing
Antibody tests look for your immune system’s response to HSV rather than the virus itself. They measure IgM and IgG antibodies, which indicate recent or past exposure.
A positive HSV-1 IgG result suggests prior infection, often oral, while HSV-2 IgG points to genital infection. These tests are most useful when no lesions are available for swabbing or when evaluating partners for exposure.
Results can take days, and early infections may not yet produce detectable antibodies. Because of this, repeat testing may be recommended after several weeks. Antibody testing helps you and your provider understand your infection history and manage future outbreaks more effectively.
Treatment and Management
You can manage herpes simplex virus (HSV) effectively with antiviral medications, symptom control, and preventive habits that reduce transmission. Consistent care helps limit outbreaks, decrease viral shedding, and maintain your overall well-being.

Antiviral Medications
Antiviral drugs form the foundation of herpes treatment. The most commonly prescribed options include acyclovir, valacyclovir, and famciclovir. These medications interfere with viral replication, reducing the severity and duration of outbreaks.
You may take antivirals in two ways:
- Episodic therapy – started at the first sign of symptoms to shorten outbreaks.
- Suppressive therapy – taken daily to reduce recurrence frequency and lower the risk of transmission.
In severe or resistant cases, intravenous antivirals or newer agents like pritelivir or amenamevir may be used under specialist care. You should always follow dosing instructions and discuss side effects such as nausea or headache with your healthcare provider.
Managing Outbreaks
When an outbreak occurs, prompt action can ease discomfort and speed healing. Begin antiviral therapy as soon as you notice tingling, itching, or burning sensations. Keep affected areas clean and dry to prevent secondary infection.
Use cool compresses or topical anesthetics (like lidocaine gel) to relieve pain. Avoid tight clothing and minimize friction on lesions. Over-the-counter pain relievers such as acetaminophen or ibuprofen can reduce discomfort and inflammation.
Tracking your triggers—such as stress, fatigue, or illness—can help you anticipate and manage recurrences. Maintaining good sleep and hydration supports your immune system and may reduce outbreak frequency.
Prevention Strategies
Reducing transmission risk requires consistent precautions. HSV spreads through skin-to-skin contact, even when no visible sores are present. Using condoms or dental dams lowers, but does not eliminate, the chance of passing the virus.
Avoid sexual contact during active outbreaks or when prodromal symptoms appear. Daily suppressive antiviral therapy can further decrease viral shedding and transmission risk.
If you have oral herpes, avoid sharing lip balm, utensils, or razors. For genital herpes, communicate openly with partners and consider joint testing to understand each person’s HSV status.
| Preventive Measure: Daily antivirals | |
|---|---|
| Effectiveness | High |
| Notes | Reduces recurrences and viral shedding |
| Preventive Measure: Condom use | |
|---|---|
| Effectiveness | Moderate |
| Notes | Lowers but does not remove risk |
| Preventive Measure: Avoiding contact during outbreaks | |
|---|---|
| Effectiveness | High |
| Notes | Prevents direct exposure |
Living with Herpes
A herpes diagnosis can feel overwhelming, but with proper management, you can lead a full and healthy life. Outbreaks often become less frequent and milder over time.
You may find emotional support through counseling, support groups, or talking with trusted friends. Open communication with partners builds understanding and reduces stigma.
Focus on maintaining your general health. Balanced nutrition, regular exercise, and stress management all strengthen your immune response. Remember that herpes is common and manageable, and with consistent care, you can minimize its physical and emotional impact.

Vaccination Program
Explore our range of vaccination programs designed for your specific health needs.

