Male hormones influence far more than just reproduction—they control muscle development, bone density, mood, and even cognitive functions in men. These chemical messengers, known as androgens, are responsible for the development of male characteristics and regulate key bodily functions from youth through old age.
Testosterone is often the focus of discussion, but the male hormonal system involves a complex network of different hormones. Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland control testosterone production, while dihydrotestosterone (DHT) performs specific functions in the skin and prostate.
A balanced hormonal level is crucial for a man’s physical and mental well-being. Imbalances can lead to various symptoms, ranging from decreased libido and muscle loss to mood swings.
Key Takeaways
- Male hormones regulate sexual characteristics, muscle development, bone density, and psychological well-being.
- Testosterone, LH, FSH, and DHT work in coordination to control various bodily functions.
- Hormonal balance is essential for the physical and mental health of men.
Contents
- Definition and Overview
- Important Groups: Androgens and Sex Hormones
- Regulation of Hormone Production
2. Key Male Hormones and Their Functions
- Testosterone: The Primary Androgen
- Dihydrotestosterone (DHT) and Its Effects
- Other Androgens: DHEA, Androstenedione, and Androsterone
- Metabolism and Distribution in the Body
What are male hormones
Male hormones are chemical messengers that control specific bodily functions and regulate male development. These androgens are primarily produced in the testes and controlled by the pituitary gland.
Definition and Overview
Male hormones are chemical compounds that regulate a variety of functions in the male body. They ensure that the body develops correctly and remains in a functional state.
Androgens represent the most important group of male hormones. These sex hormones are primarily formed in the testes, but are also produced in small amounts in the adrenal glands.
These hormones influence not only physical development but also psychological functions. They regulate memory, concentration, and mood in men.
Male hormones also exist in the female body, but in significantly lower concentrations. This small amount fulfills important physiological roles in women.
Important Groups: Androgens and Sex Hormones
Androgens form the main category of male sex hormones. Testosterone is the most well-known and most important androgen in the male body.
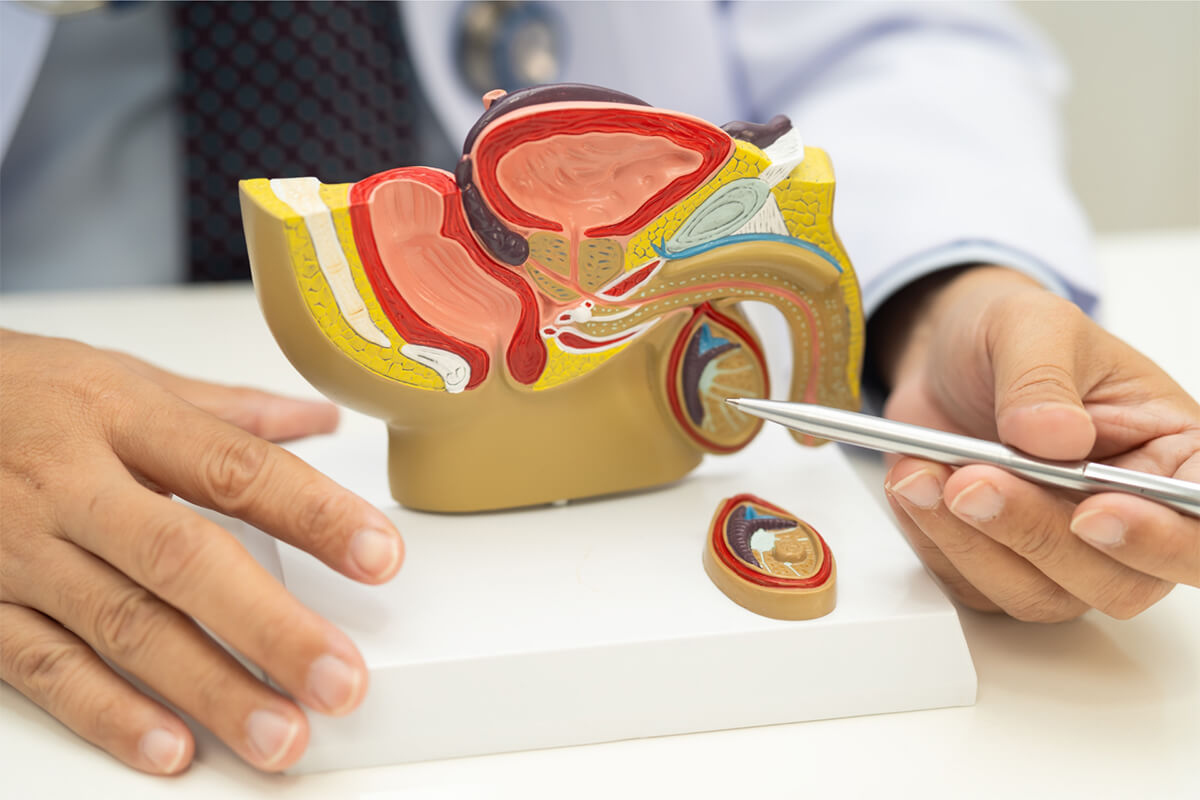
Testosterone is mainly produced in the Leydig cells of the testes. It is responsible for the development of secondary sexual characteristics such as body hair, a deepening voice, and muscle development.
Dihydrotestosterone (DHT) is created through the conversion of testosterone with the help of the enzyme 5-alpha-reductase. DHT influences hair growth, skin functions, and prostate health.
Other important hormones include luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These are produced in the pituitary gland and control testosterone production as well as sperm maturation.
Regulation of Hormone Production
The pituitary gland acts as the central control unit for male hormone production. It produces LH and FSH, which act directly on the testes.
Luteinizing hormone stimulates the Leydig cells to produce testosterone. A complex feedback mechanism continuously regulates this hormone secretion.
FSH acts on the Sertoli cells in the testes. These cells support sperm development and maturation in the seminiferous tubules.
Hormone regulation occurs through an interplay between the hypothalamus, the pituitary gland, and the testes. Disruptions in this system can lead to hormonal imbalances and fertility problems.
Key Male Hormones and Their Functions
Male hormones form a complex system of various androgens, each undertaking specific tasks within the body. Testosterone functions as the primary hormone, while DHT, DHEA, and other androgens fulfill supplementary roles and are distributed throughout the body via precise metabolic processes.
Testosterone: The Primary Androgen
Testosterone is the most important male sex hormone, with approximately 95% produced in the testes. The adrenal glands contribute the remaining 5%.
The normal testosterone level in healthy men ranges from 300-1000 ng/dl. These levels naturally fluctuate throughout the day, with the highest concentrations occurring in the morning.
Key functions of testosterone:
- Development and maintenance of male reproductive organs
- Promoting muscle growth and bone density
- Regulating libido and sexual function
- Stimulating sperm production
- Controlling body hair and voice depth
Testosterone circulates in the blood in three forms: about 2% as free testosterone, 44% bound to albumin, and 54% bound to SHBG (Sex Hormone-Binding Globulin). Only the free and albumin-bound testosterone are biologically active.
With increasing age, testosterone levels decrease by approximately 1-2% annually. This natural decline typically begins around the age of 30.
Dihydrotestosterone (DHT) and Its Effects
DHT is formed from the conversion of testosterone by the enzyme 5α-reductase. Although present in smaller quantities, DHT is biologically about 2-3 times more potent than testosterone.
Primary effects of DHT:
- Development of external genitals during the embryonic phase
- Prostate growth during puberty and adulthood
- Development of male body hair (beard, body hair)
- Regulating hair growth on the scalp
DHT is primarily produced in the skin, prostate, and hair follicles. The highest concentrations are found in these target tissues.
An excess of DHT can lead to prostate enlargement and androgenetic alopecia (male pattern baldness). Certain medications can inhibit DHT production to reduce these effects.
The DHT concentration in the blood is normally about 10% of the testosterone level. Despite this lower concentration, DHT plays a crucial role in male development.
Other Androgens: DHEA, Androstenedione, and Androsterone
DHEA (Dehydroepiandrosterone) is mainly produced in the adrenal glands and serves as a precursor to other sex hormones. DHEA levels peak around the age of 25 and decline continuously thereafter.
DHEA’s functions include supporting the immune system, regulating energy metabolism, and providing the building blocks for testosterone and estrogen.
Androstenedione functions as a direct precursor to testosterone and estrogen. It is synthesized in both the testes and the adrenal glands.
The concentration of androstenedione is significantly lower in men than in women. It plays an important role as an intermediate step in hormone production.
Androsterone is a metabolic byproduct of testosterone and DHT. It possesses weak androgenic properties and is primarily excreted through urine.
These hormones work together synergistically, influencing various aspects of male physiology and development.
Metabolism and Distribution in the Body
Androgen metabolism begins with cholesterol as the starting molecule. Through several enzymatic steps, DHEA and androstenedione are formed first, which are then converted to testosterone.
Metabolic pathways of androgens:
- Cholesterol → Pregnenolone → DHEA → Androstenedione → Testosterone
- Testosterone → DHT (via 5α-reductase)
- Testosterone → Estradiol (via Aromatase)
The liver plays a central role in hormone breakdown. Here, androgens are converted into water-soluble metabolites and excreted via urine and bile.
Transport proteins in the blood:
- Albumin: Binds approximately 44% of circulating testosterone.
- SHBG: Transports 54% of testosterone with high affinity.
- Free Hormone: Only 2%, but it is the most biologically active.
The half-life of testosterone in the blood is relatively short, typically ranging from 10 to 100 minutes, which reflects its rapid metabolism and clearance from the body.
The Role of Male Hormones in the Body
Male hormones control sexual development from puberty into adulthood and regulate sperm production in the testes. They directly influence libido, sex drive, and erectile function, as well as the development of physical traits like body hair and voice pitch.

Sexual Development and Reproductive Function
Testosterone initiates male sexual development in the womb and continues it during puberty. The hormone causes the growth of the penis and testes and the development of secondary sexual characteristics.
In the testes, testosterone stimulates sperm production by the Sertoli cells. This process takes about 74 days and requires consistent hormone concentrations for optimal fertility.
Reproductive function depends on several androgens. Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) regulate testosterone production and spermatogenesis.
A testosterone deficiency can lead to reduced sperm quality and count. This significantly impairs male fertility and can cause infertility.
Influence on Libido, Sex Drive, and Erectile Function
Testosterone directly regulates sex drive and libido in men. Low hormone levels often lead to diminished sexual interest and reduced sexual activity.
Erections are controlled by complex hormonal mechanisms. Testosterone influences blood flow to the penis and the function of the smooth muscle in the erectile tissues.
Dihydrotestosterone (DHT) enhances the effect of testosterone on sexual function. It binds more strongly to androgen receptors than testosterone itself.
A hormone deficiency can lead to erectile dysfunction. Affected men often report weaker or less frequent erections, especially with age-related testosterone decline.
Physical Characteristics and Hair Growth
Male hormones shape characteristic physical features. Testosterone promotes muscle growth, bone density, and the typical male body shape with broader shoulders.
Body hair develops under the influence of androgens. During puberty, testosterone and DHT stimulate hair growth on the chest, face, arms, and legs.
Paradoxically, hair loss is caused by the same hormones. In genetically predisposed men, DHT shortens the growth phase of scalp hair, leading to androgenetic alopecia (male pattern baldness).
The voice is influenced by testosterone. The hormone causes the larynx (voice box) to grow and the vocal cords to thicken, resulting in a deeper voice pitch.
Effects on Mood and Behavior
Testosterone significantly influences mood. Normal hormone levels promote self-confidence, motivation, and emotional stability in men.
A testosterone deficiency can lead to depression, irritability, and a lack of drive. Those affected often report fatigue, concentration problems, and a reduced enjoyment of life.
Behavior is modulated by androgens. Testosterone can enhance competitive behavior and assertiveness without necessarily promoting aggression.
Men’s health benefits from balanced hormone levels. Testosterone supports mental health and contributes to a stable emotional equilibrium.
Hormonal Balance and Men’s Health
Hormonal balance influences male health in numerous ways. Testosterone deficiency leads to physical and psychological issues, while the age-related decline in hormones brings about inevitable changes.

Testosterone Deficiency and Symptoms
Testosterone deficiency affects various bodily functions and is identified by characteristic signs. Diagnosis is made through blood tests and a clinical evaluation of symptoms.
Physical Symptoms:
- Decrease in muscle mass and strength
- Increase in body fat
- Reduction in bone density
- Fatigue and lack of energy
Psychological Effects:
- Mood swings
- Irritability and depression
- Difficulty concentrating
- Decreased self-confidence
LH (Luteinizing Hormone) levels often rise when the testes do not produce enough testosterone. This indicates a primary testicular dysfunction.
Aging and Changes in Hormone Levels
Starting around the age of 30, testosterone levels decrease by approximately 1-2 percent annually. This natural decline leads to various age-associated changes.
The hormonal decline is gradual and differs from the abrupt menopause experienced by women. Men do not experience a complete cessation of hormone production.
Age-related changes:
- Reduced libido
- Slower recovery after physical exertion
- Altered sleep patterns
- Decline in cognitive performance
Hormone production in the testes decreases, while other hormones like cortisol often remain elevated. This worsens the hormonal imbalance in old age.
Connection to Prostate Health and Infertility
The ratio between testosterone, estrogens, and other hormones significantly influences prostate health. An imbalance can lead to an enlarged prostate or other issues.
Hormonal influences on the prostate:
- Testosterone is converted to dihydrotestosterone (DHT)
- DHT stimulates prostate growth
- Estrogens can promote inflammatory processes
Several hormonal factors play a role in infertility. Testosterone deficiency directly reduces sperm production and quality.
LH and FSH (Follicle-Stimulating Hormone) regulate testicular function. Disruptions in these hormones impair both testosterone production and spermatogenesis (sperm development).
Treatment requires a precise hormone analysis. Therapeutic measures must consider the entire hormonal network, not just individual hormones.

